A recent article published by MedPage Today and KFF Health News sent my brain into orbit. Entitled, Amid Falling Diversity at Med Schools, a Warning of DEI Crackdown’s Chilling Effect, the sub-title noted, “Education and health experts say this could ultimately harm patient care”. Use of “Could” in light of overwhelming evidence infuriates me. There is no “could” about it; the current DEI crackdown in academia will yield negative outcomes for the workforce, but also worsen the quality of care rendered to patients, their families, and the communities we serve.
The Value of Concordant Care
Concordant care involves aligning treatment with patient values and preferences. It is demonstrated in many ways, from open communication to having providers of the same race, ethnicity, sexual orientation, as well as gender identity, or gender expression. As a result, patients and their families feel psychological safety within a practice setting. Empathy is a vital competency for every healthcare professional that should be demonstrated toward every patient. But the ability to do so does not always assure concordant care. This is especially true when practitioners are employed by larger healthcare systems and organizations.
A patient’s need for health and behavioral health treatment brings them to practitioners for care. Yet, it is a patient’s trust in these practitioners that fosters their engagement in the care process. In addition, a patient’s comfort with providers of the same ethnicity, gender, race, or life experiences promotes their ability to feel safe, seen, heard, valued, and respected in the treatment space. In tandem, the practitioner’s knowledge of a patient’s culture, values, and beliefs inform their awareness of patient health literacy opportunities. This might translate to addressing spiritual and cultural differences in care, such as the need for prescription medications or treatments for chronic illness or even behavioral health.
Discordant care contributes to medical gaslighting and invalidation. Dismissal of the patient and caregiver voice is the top patient safety issue for 2025, and a frightening fact. Increased numbers of Black primary care physicians are associated with longer life expectancy and lower mortality rates among Blacks. Similarly, when providers can identify with their patients, there are higher degrees of patient engagement, patient satisfaction, and treatment adherence for women, members of the LGBTQIA+ community, and other traditionally marginalized groups.
Healthcare utilization is higher and care costlier for these populations due to a trail of ignored complaints and symptoms and missed diagnoses. Their mortality rates are upwards of double that of numbers for less marginalized groups. These figures will only worsen as the patient voice is reduced, and particularly for traditionally marginalized populations and communities. My prior articles have detailed these abysmal numbers, with an upcoming article on this topic to be published in the May/June issue of Professional Case Management.
Systemic Bias
Countless thought leaders have emphasized the need for attention to treatment bias in healthcare. The Institute of Medicine’s seminal 2003 report, Unequal Treatment noted how African Americans and those in other minority groups receive fewer procedures and poorer-quality medical care than Whites. Stereotypes and stigma have impacted care across every cultural nuance encompassing ethnicity, gender, disability, race, and sexual identity to name just a few. These faulty beliefs have impacted every aspect of care from inaccurate treatment algorithms that fail to account for gender, race, and ethnicity to effective pain and other symptom management. Proper prescription medication dosing and other treatment is also at issue with condition not properly addressed. Patients are unnecessarily blamed for their symptom presentation rather than being fully assessed for individualized care.
The Mandate for Workforce Diversity and DEI Programs
A series of professional reports have identified opportunities to advance diversification of the healthcare workforce. The Council on Social Work Education revealed while 90% of social workers graduating with their MSW were women, opportunities for enhancing diversity continue to present. Only 22% of these same students were Black and 14% were Hispanic or Latino. The National Council of State Boards of Nursing revealed similar numbers with nurses from minority backgrounds representing under 20% of the RN workforce. Composition with respect to racial backgrounds is:
- 80.6% Caucasian
- 6.7% African American
- 7.2% Asian
- 5.6% Hispanic
- 0.5% American Indian/Alaskan Native
- 0.4 Native Hawaiian/Pacific Islander
- 2.1% two or more races; and
- 2.5% other
The Physician workforce also fails to reflect the inclusive nature of patient populations:
- White: 56.5%
- Asian: 18.8%
- Hispanic or Latino: 6.3%
- Black or African American: 5.2%
- Multiracial (non-Hispanic): 1.3%
- Other: 1.1%
- American Indian or Alaska Native: 0.3%
- Native Hawaiian or Other Pacific Islander: 0.1%
- Unknown: 10.4%
Gender composition notes a greater percentage of those identifying as male vs. female: 60.5% compared to 39.5%.
There is growing availability of health and behavioral health professionals who provide affirming, accepting, and inclusive care to all patients, yet access remains challenging. Outcare and FOLX health provide directories of LGBTQIA+ friendly providers. Data detailing workforce composition for this community remains limited, though one report notes barely 14% of all medical students identify within the community.
In direct response to the percentages above, professional schools advanced DEI programs. Academia has worked for the better part of the last decade to shift from a curriculum of racial bias and develop antiracist and anti-oppressive programming. New coursework was developed with expansion of learning experiences, practicums, residencies, and specialized learning forums. These approaches prepared clinicians to better understand the patients they treat. Deshazo et al. (2021) identify how “deeply rooted bias is within the infrastructure of American Medicine, based on skin color, religion, immigrant status, gender, and ethnicity are deeply rooted, and taught as scientific racism medical schools from their earliest points in history.” This new societal playbook is a return to those times where fear of segregation and rampant inequities in access to quality care are the norm, along with putting minorities and women “back in their place”.
The UC Davis School of Medicine initiated a “race-neutral, holistic admissions model”, which tripled enrollment of Black, Latino, and Native American students. Assorted other efforts increased funding and entry to healthcare career pathways for students unable to otherwise afford or access them. There are an endless list of merits for the communities served by these new clinicians, including growth of diverse workforce that matches the patients served.
Communities Take Care of Their Own
I’ve long said that communities take care of their own and this reality can’t be overstated. Practitioners of color are more likely to build their careers in medically underserved areas, from rural communities to lower socioeconomic areas. The 2024 report by AAMC is clear: a shortage of >40,00 primary care doctors is expected by 2036 unless dramatic changes occur.
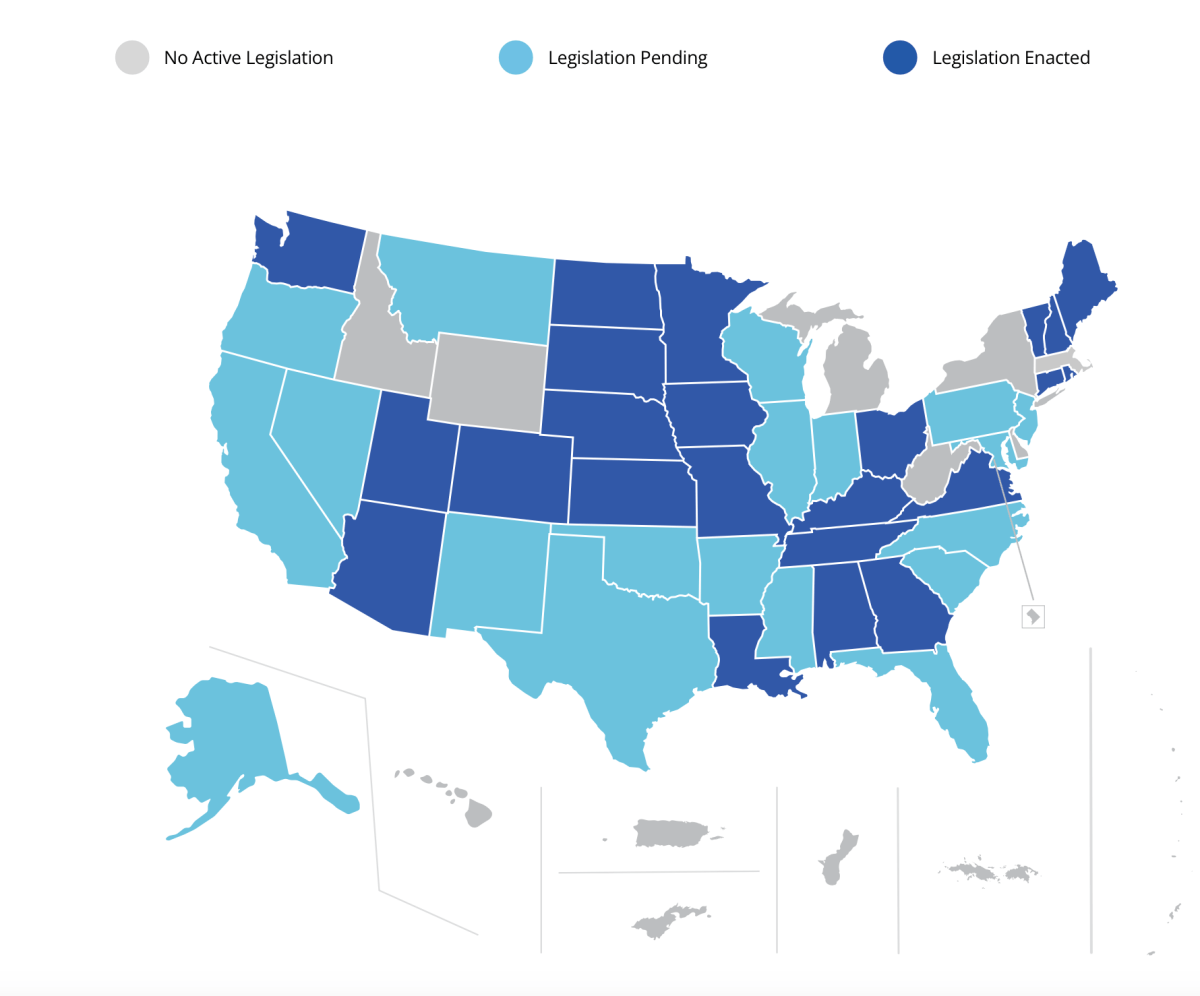
One way to assure workforce intercultural effectiveness has been through CEU-requirements for licensure and renewal. Yet even these requirements are now at risk. The Texas Behavioral Health Executive Council voted for removal of language requiring cultural competence as a CEU-requirement for licensed mental health professions with other states working to advance similar actions. This move de-emphasizes cultural context as a critical element of providing and assuring ethical and responsible care and intervention to each person. These shifts will create gaps in the knowledge and skills needed for the workforce to effectively engage with and serve patients from diverse backgrounds, cultures, and genders. Respect for the unique experiences, beliefs, and values that distinguish populations and communities will surely be at risk.
Moving Forward
As my colleagues in this space know, strategic action remains a moving target. We stay informed, yet angry at the daily assault on inclusion. Yet, that anger drives my actions, which are absolute:
- I stay committed to the Quintuple Aim: providing patient- and family-inclusive care at the right time, right cost, rendered by those who embrace the work, and ensuring equity and accessibility for all.
- I continue to heed my professional ethical obligations to patients, their families, and colleagues. Every day, I define one tangible way to step up in this shifting space to advance diversity, equity, inclusion, accessibility, belonging, and social justice, and through my every action, whether by:
- Use of my professional voice through teaching, training, or authorship.
- Supporting the workforce through ethical challenges faced in their workspaces.
- Mentoring newer practitioners on clear strategies for their own sustainability.
- Advocacy through my assorted roles across the industry
- I continue to heed my professional ethical obligations to patients, their families, and colleagues. Every day, I define one tangible way to step up in this shifting space to advance diversity, equity, inclusion, accessibility, belonging, and social justice, and through my every action, whether by:
How will you step up and into this space today?