It’s that time of year when my Master’s in Social Work students are graduating. They are ready to be done with the academic rigor and make their unique mark on the industry. Of course, they also want to obtain gainful employment that values their education and their coveted degree.
My biggest hope is that all of my students find their dream job, and especially my Masters’ folks. They struggle the most in accessing jobs aligned with their interests, salary requirements, as well as providing them quality social work supervision toward licensure. The role should also provide them psychological safety and prioritize their professional self-care, not to mention a few other things.
How do you engage in a successful job search? How and what do you negotiate? Who’s interviewing who on the interview? Here are 15 lessons to activate and succeed in your job search! While the focus of this blog is vital for MSWs, there is valuable information for all job searchers in this space.
Lesson 1: Organize
Set up an electronic folder on your computer with subfolders:
· References
· Cover letters
· Interview questions
· Submitted applications
· Recruiter contacts
· Key info about jobs applied for
Track positions on a spreadsheet with information including application dates, if you heard back and when, job details (e.g., salary, key benefits, virtual or in-person, multiple sites), contact information. I’m a fan of Excel, but how to organize is up to you!
Lesson 2: Keep your resume focused, comprehensive, and competency-based.
A resume is your professional face. In your zest to post and send it to potential employers, it becomes easy to include too much info, be too wordy, or use unprofessional language. Think:
· Formatting: Use a resume template, plus career planning offices at your academic institution, as well as:
–Beamjobs
–Indeed.com
–The New Social Worker
–ResumeGenius
More folks are using AI to build their resumes, so here are several established resources:
–Canva AI Resume Builder
–Resume-Now
-MyPerfectResume
· Use competency-based language: Professions have competencies that are viewed as the pillars of practice. Use that language to describe roles for practicums, internships, or professional jobs; for example, ‘intervened with adolescent population’ instead of ‘worked with adolescents’. Another example is, ‘engaged in counseling’ instead of ‘provided, or did counseling’. Competency-based language also lives in course syllabi and licensure regulations for your state.
· Attention to detail matters: A resume is your first impression to prospective employers. If there are errors, they will wonder, ‘if you can’t take the time to proof your own resume, why should they believe you’ll do better on the job?’. Do spelling AND grammar checks!
Lesson 3: Have references ready!
Reach out to references early and keep their current contact information accessible. Maintain professional letters of recommendation in your online files. Keep your references in the loop so they know to expect contact by a potential employer. It also helps to share with your references if you really want that job. With so many phishing emails, everyone is cautious about providing information. Your reference can easily miss a vital request to provide the recommendation that leads to a job offer!
Lesson 4: Know what matters to the organization
This lesson is two-fold: first, keep up on public health facts and their impact for populations served by the agency. Brush up on Crisis theory, Intersectionality, Trauma-informed care, and short-term counseling techniques. This info will help you develop ideas on how to best serve the organization. Knowledge is power; this is a great way to tout your expertise in the interview.
Second, ask how the organization continues to address DEIB-related (Diversity, Equity, Inclusion, and Belonging), as well as how they refer to these concepts. These values continue to underlie social work practice. The information goes beyond what may be on the employer’s website. You want to know exactly what mechanisms are in place to ensure all employees, patients/clients, their families and other strategic partners feel safe, seen, heard, and valued, and through every aspect of care and organizational operations.
Lesson 5: Know brief assessment tools and resources
With the uptick in mental health across populations and the workforce, have working knowledge of assessment tools to manage anxiety, stress, and depression. Know how to develop SMART goals as well! Quality resources continue to live at Therapist Aid and AHRQ
Lesson 6: Interviews are reciprocal opportunities
Interviews are not a guarantee of employment. Candidates can spend so much time during an interview discussing their expertise, they forget to ask key questions about the workplace.
Research employers before the interview. View the employer’s website to learn their mission, vision, and goals. Learn how the organization conducts business. Ask questions about short and long term goals and how they see you fitting into these plans. This tactic conveys your interest in the position.
Keep in mind that while interviews are for potential employers to interview you, you also get to interview them. This mindset puts you in control of the process, and decreases anxiety. Ask questions to learn if this job and setting are for you, such as those at Big Interview.
Remember, decision-making timeframes vary, so ask about next steps. Organizations can take 2 days to make final decisions or months! Know what you are facing to help prioritize other offers!
Lesson 7: Ask about job stability
Amid these unpredictable times, it’s appropriate to ask about potential layoffs and furloughs. Some positions are funded by grants, so ask how long the position is funded and what happens next. Hiring freezes may happen and won’t necessarily be information shared. If you don’t ask, you won’t know.
Lesson 8: Be ready to name your unique strengths, and demonstrate them
Job candidates will be asked how to handle specific situations. Identify your strengths and how they would make a difference. Consider:
· How do your strengths set you apart from other candidates?
· Why should the organization hire you?
· What examples can you provide so the employer understands your worth?
· How can you demonstrate your ability to work with a team?
· You will be asked about your weaknesses. Be prepared to respond in a professional manner, and have your answer ready.
Lesson 9: The only constant in our industry is change
You may be happy to be done with school, but must still be open to new learning: the industry will change as will you. Be open to what it means for you to change with it.
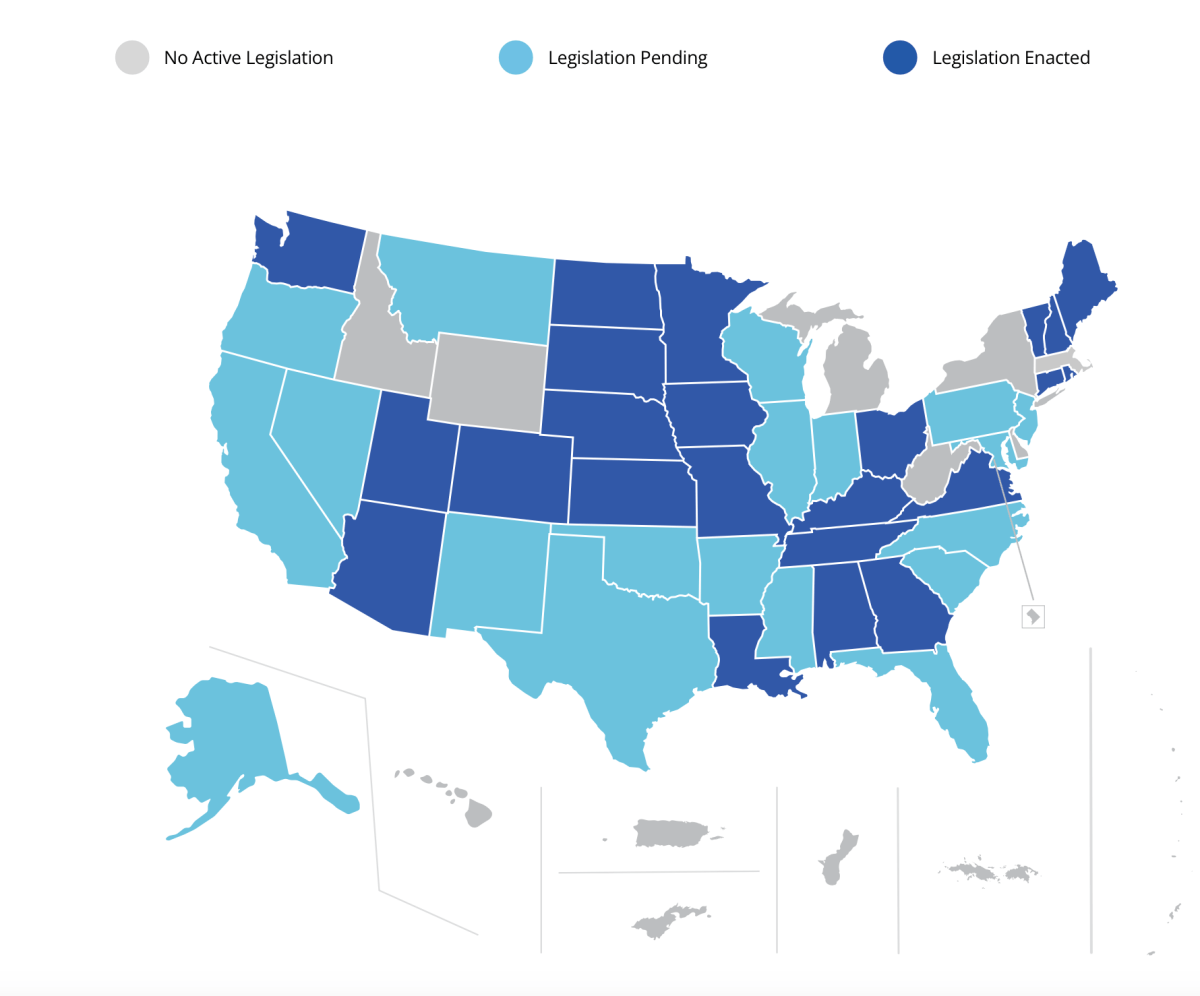
One big area of change for licensed health and behavioral health professionals involves licensure compacts and the ability to practice across state lines. Stay informed on the scope of practice within your state, and advancement of the Social Work and other Compacts.
Lesson 10: Be open to short-term or part-time roles
An exciting short-term or part-time role may turn into the best career option never anticipated. More and more MSWs are accepting multiple part-time roles. These options can promote greater flexibility, while minimizing burn-out. Also, don’t dismiss positions that are different from your expectations!
Lesson 11: Set up your professional social media profile.
Set up a professional profile using established websites and job bank platforms. Facebook (or Meta) can help with networking, but use other websites that highlight recruitment:
Keep a profile professional! Use a polished photo versus a selfie with your BFF, pet, or family! Solid guidance is at The Ultimate Guide to Crafting a LinkedIn Profile that Recruiters Love
Lesson 12: Negotiation is expected
Negotiation is expected for any job. Negotiate for everything:
- A higher hourly rate or salary
- Remote options or flexible work hours
- Coverage/reimbursement for professional fees (e.g. licensure exam application, exam prep courses, professional association dues)
- Coverage/reimbursement for clinical supervision and if it is offered as an employment benefit. Organizations may pay a portion of the rate to the whole amount. They may only provide supervision internally or have waiting lists (so, YES, ask how long the waiting list is!). If supervision is provided, you may need to promise to stay at the organization for set number of years post-completion and attainment of your licensure. Otherwise, you may need to pay pack a set amount.
- Don’t forget to ask if the organization has clinical social work supervisors employed by the agency (and who’s met any state requirements) and their availability. It can take some time to find that supervisory “goodness of fit”, knowing sooner than later is better.
You don’t know what you don’t know, so ask questions! The answers may surprise you!
Lesson 13: Don’t be thrown by a title or position qualifications
People apply for jobs based on titles; titles are deceptive! Learn about the scope of each role before dismissing a solid opportunity.
Don’t dismiss a role based on qualifications alone. Application processes may ‘kick you out’ for not having hard competency qualifications (e.g., degree, licensure). Other knowledge or experiences can sway the decision; volunteer roles and practicums with a population speak volumes. Don’t assume you’re not qualified!
Lesson 14: Take the right job, not just any job
You want an income when you graduate, but strive for the right job. Listen to your clinical gut during the job search. Don’t jump on the first offer or settle if something feels off. Process the opportunity with peers, former professors, and mentors. Remember, the grass isn’t always greener elsewhere; there are brown spots everywhere.
Lesson 15: Enjoy the job search
There is pressure to be employed, but explore opportunities to fine the right one for you. Get out there and enjoy the search!
I invite colleagues and followers to post other practical lessons below to empower our next generation of professionals!