First, big thanks to all who read my last blog post Health Equity and the SDoH are Not Synonyms. That article has quickly become my top blog post with thousands of views across social media platforms and other news outlets. Ellen’s Interprofessional Insights is free access to all who value its messaging, so please share the link. Now, onto my latest fierce focus.
I was reminded last week of a long-standing pet peeve: (mis)use of the terms compliance and adherence. I participated in RISE’s Annual Population Health Summit with vibrant conversations int he space about patient engagement. Through a number of sessions there was THAT framing that makes me vibrate with frustration. My brain went into overdrive!
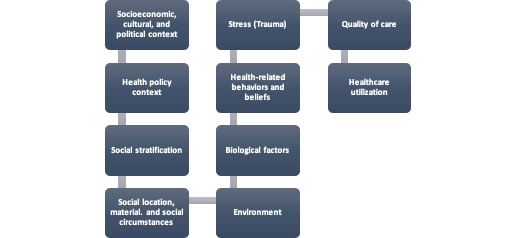
When will the industry stop blaming patients for treatment inactions? Has there not been enough focus on DEI strategies to enhance practitioner and provider cultural awareness and humility? How much emphasis has there been to advance assessment of health-related social needs (HRSNs) or social drivers of health, patient health literacy, and decreasing biases? (Psssst: Remember, the CMS penalties and Joint Commission standards (TJC) are real!). Despite a resounding YES to the above questions, we’ve got miles to go before we sleep. Use of the term “compliance” instead of “adherence” by healthcare regulatory entities and organizations, plus practitioners, health systems and their and employees only condones the blaming of patients for poor outcomes. It’s time to change this practice!
Compliance Conveys Power Not Partnership
I’m notorious for level-setting and wanted to start with a review of definitions. Compliance refers to regulatory enforcement of applicable requirements whereby organizations and their providers are expected to meet or exceed the defined legal, ethical, and professional standards.Their explicit goal is to reduce fraud, abuse, and waste, with the implicit intent to ensure patient and occupational safety. Yet, there is a concerning power dynamic imposed by this definition as regulatory entities (e.g., NCQA, NQF, TJC) possess legitimate power by virtue of their role in the industry.
Compliance also implies power verses partnership. The term speaks to an assumption that patients must be subservient to a practitioner’s authority, a troublesome concept for this clinical professional. What happens when a patient’s voice is not heard or dismissed by practitioners? What about when a patient doesn’t feel seen? These situations emerge with increasing incidence across every population, with who are marginalized and minoritized experiencing this reality in unacceptable numbers.
Compliance suggests passive behavior, as when a patient is expected to follow treatment instructions. It may be the patient who is comfortable doing what the physician tells them to, whether take a prescribed medication in a defined dose or follow-up for counseling with a behavioral health provider. Some patients may heed this guidance as the norm, not daring to question their provider, while others will seek to clarify the rationale. This approach should not be surprising in an era where patients are consumers of their care. However, questioning, challenging, or ignoring provider recommendations is too often viewed as a negative.
Power and misused power yield trauma, whether historical, experiential or event in scope. Acute, chronic, and complex trauma share misused power and/or oppression at their source. Blaming patients is laden with stigma and accusatory messaging. It gets me wondering how much attention is paid to a patient’s health literacy, language proficiency, or any of their concordant preferences.
By contrast, adherence is the active choice of patients to follow through with prescribed treatments, while taking responsibility for their well-being. This term signifies that patients and practitioners collaborate to improve their health behaviors toward overall a higher state of wellness. Successful outcomes are achieved through a blend of clinician expertise with patient choice incorporating lifestyle, values, and care preferences. Shared decision-making and personal integrity leverage meaningful therapeutic relationships.
Sync for Social Needs, Z-Codes, Yet Being Out of Sync
I was excited when NCQA, NQF, and the TJC joined the Sync for Social Needs Coalition. Yet, these entities present as out of sync with their views on how to best assess and address exactly what drives patient motivation and engagement in treatment. NCQA still uses the term adherence on their resource pages and metrics. TJC echoed emphasis on patient activation and adherence in recent issue briefs.
My beloved Z-Codes are not so in sync either. ICD-10-CM Z codes for Patient Noncompliance were expanded in 2023 to my disappointment. To be fair, I’m a member of the Gravity Project and tout their work at every opportunity. However, I took a brief break from my involvement to finish my Doctoral Culminating Project. The mantra, you snooze, you lose applies!
Z-Code Z91.1 of patient noncompliance with medical treatment and regimen made me shiver. How is this concept objectively evaluated in the current care climate? Hearing colleagues refer to “non-compliant patients” always felt subjective. The terminology stirred thoughts of misbehaving children or those unable to follow traditional societal norms.
My clinical training aligns with psychodynamic theory, thus there are always reasons for all behaviors, whether conscious or unconscious. This approach explains why a person may present as unable or unwilling to follow medical treatment. If we don’t ask why, we can’t properly assess the reasons for these behavioral manifestations. Expanding these codes gave the industry license to label patient actions as “noncompliance” with their dietary regimen and medical treatment. Caregivers of patients are also subject to these same biasesfor their “noncompliance “with an expansive list of codes under Z.91. These codes can be viewed here.
This terminology use is shocking given how the workforce is readily cued to manage their biases, stay informed of microaggressions, and participate in continuous learning to decrease missteps. Training on cultural awareness to promote patient engagement and satisfaction with care is emphasized at every turn. Yet, I am disappointed that practitioners are empowered to code, and thus blame, patients and caregivers for treatment disparities and misunderstandings.
Activating Change
Industry prioritization of health equity mandates a cultural shift in treatment language and perspectives. Here are tangible recommendations:
1. Shift the narrative and power dynamic: Practitioners and providers must shift from viewing compliant and “obedient” patients to persons provided the respect and space to partner in their treatment decisions. Autonomy and self-determination remain enduring ethical principles and amplify attention to cultural perspectives.
2. Coping with the human condition is universal: Most patients and their caregivers experience fear and anxiety about their health conditions and those of their loved ones. A majority worry about diagnosis, prognosis, and quality of life. Everyone uses some defense mechanism to cope or not (e.g., denial, isolation, projection, displacement). The reality of the health experience often occurs without warning, and usually when least expected. We must give people the grace and space to cope with it.
3. Engage to understand patient and care giver rationale: To embrace cultural awareness and humility we must seek to understand patient and caregiver behaviors. We must eliminate implicit biases rather than empower them through quality metrics and measures; “these biases reinforce blame on the patients rather than look to the system and/or the competencies of the clinicians”; big nod to my friend Michael Garrett for this quote!
4. Assess for Psychosocial Needs: This arena is a top priority for organizations and most I know are on the case to integrate reflective screening tools into their efforts. I appreciate that far more resources are needed for all of those who need them. However, let’s make sure the right team members are employed for assessment and referral of patients, including community health workers, case management assistants, and health service coordinators. The outcomes are clear about their merits to assess across the touchpoints of care for:
- Health and digital health literacy
- Cultural preferences for treatment (e.g., medication, provider gender)
- HRSNs, financial, and other impediments to care (e.g., co-pays, medical debt, lack of family support, isolation, transportation, incarceration, techquity)
5. Use Non-Judgmental Communication: It is critical we set an inclusive tone to care, including but not limited to:
- Maintain an affirming presence to establish trust
- Ask the patient to verify their gender and pronouns
- Ask the patient to verify their race and ethnicity
- Ask the patient to identify their family or support system, regardless of blood relation
- Demonstrate empathic and reflective listening
- Respect client autonomy by allowing the person to speak
- Empower patient through use of open-ended questions, such as, ‘What matters most to you?” or “What can I do for you today?”
- Respond, clarify, and confirm, instead of reacting
- Honor the patients religious and cultural beliefs, values, and choices
(Fink-Samnick & Garrett, 2023)
Unconditional respect between patients and providers is difficult, but not impossible. Little will change toward engaging patients in their needed care until we stop blaming them for the industry’s shortcomings.